Repair, Regrow, Regenerate
Lizards can regrow their tails and crabs their severed claws. Now, after decades of research, scientists including Samuel Stupp ’77 PhD are closer than ever to unlocking the human body’s healing powers.
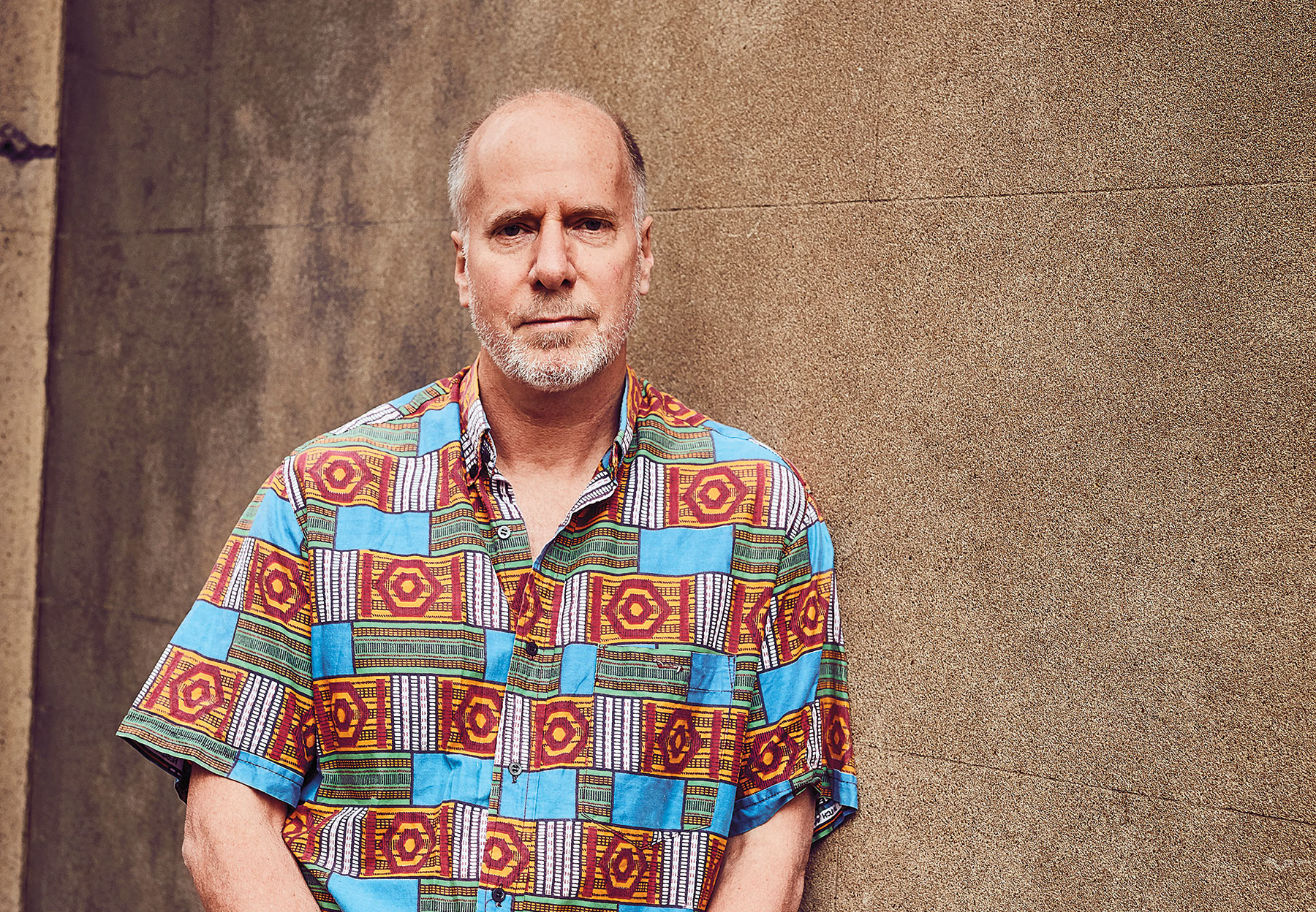
Daniel Bausch says the solution to containing infectious disease outbreaks is to win people’s trust. By Lisa Stein
Last summer international aid workers began descending from Soviet-era helicopters into the forests, mountains and villages in the Democratic Republic of Congo’s North Kivu region, setting up treatment centers and laboratories, and donning hazmat suits as they treated people sick with the Ebola virus. The workers brought computers, lab equipment, vaccine doses and anything else that supported epidemiology, data and patient management, and infection prevention and control.
And in this particular Ebola outbreak, they also brought helmets and flak jackets, courtesy of the United Nations.
Health workers in Congo have met not only disease but also a complex and often violent sociopolitical environment in communities that have suffered unimaginably for many years, at first from Congo’s civil war that killed more than 5 million people and, in recent decades, from scores of holdover armed militias, locally called Mai-Mai.
Although Daniel Bausch ’83, an expert in tropical and infectious diseases, has worked in many Ebola outbreaks, this situation seems particularly dire. Mai-Mai — intent on extorting money — and victims’ grief-stricken families attacked five Ebola treatment centers in February and March, burning down one and killing two people, causing the humanitarian organization Doctors Without Borders (Médecins Sans Frontières or MSF) to temporarily withdraw its staff.
Violence continued into the spring, when armed men stormed into an Ebola meeting in the town of Butembo and opened fire. They killed Richard Valery Mouzoko Kiboung, an epidemiologist for the World Health Organization (WHO), and injured two other workers.
Since January, more than 85 health workers have been killed or wounded, according to the WHO, and as of June 27 more than 1,430 people had died from Ebola. It has become the second-worst Ebola outbreak in history and the first to take place in a conflict zone. Now Congo and international health officials fear that the Ebola outbreak could spiral out of control unless the violent attacks against health facilities and workers stop.
“It’s an extremely complex and volatile situation, with a fearful population sometimes violently resisting control efforts,” Bausch acknowledges. “We can’t be too judgmental about the people because they have been in this violent, very manipulated situation for a long time. Ebola is often viewed as just another weapon or means of political manipulation.”
Bausch directs the United Kingdom Public Health Rapid Support Team (UK-PHRST), the UK’s unit for outbreak response and research and one of the major groups contributing to the international response effort in Congo. The organization was established in 2016 as a collaboration between Public Health England and the London School of Hygiene & Tropical Medicine in the wake of the devastating 2013–16 Ebola outbreak in West Africa, which killed more than 11,000 before being contained. These days Bausch has given up his role as a primary care provider for Ebola patients to focus on the big picture, supervising UK-PHRST response efforts and organizing research programs. His full-time staff of roughly 30 public health experts, scientists, academics and clinicians is ready to respond to urgent requests from countries around the world within 48 hours to help prevent local disease outbreaks from becoming global epidemics.
After spending decades helping to contain viral outbreaks across Africa, Latin America and Asia, Bausch has become sure of one thing: The solution to containing infectious diseases lies in engaging communities and winning their trust. All the equipment, procedures and even vaccines won’t stop transmission if people don’t understand what the disease is and feel part of the solution.
Bausch points out that communities that experience significant Ebola outbreaks have long histories of illness, poverty and violence, and their residents have grown suspicious of international workers. In recent years, international response agencies — including the U.S. Centers for Disease Control and Prevention (CDC), the WHO and MSF — and other nongovernmental organizations (NGOs) have been changing how they approach disease-stricken places.
“Early on, international aid groups focused on the technical side of things as epidemiologists aimed to stop transmission but often overlooked the needs of the individual patient,” Bausch explains. “We would come in and say, ‘Ebola is a very dangerous disease, and it can kill you, so don’t have contact with sick people,’ and then put people in Ebola isolation units but without much explanation.”
Over the years that impersonal approach made it extremely challenging to bring a person suspected of having Ebola into a treatment center, because so many residents grew wary of bringing family members to a facility into which they disappeared and didn’t return.
“If people don’t understand what’s happening and think that they’re just going to a facility to die, why would they go?” Bausch asks.
Now those same agencies have developed protocols that call for making treatment centers more welcoming and less frightening. Rather than immediately placing patients in isolation, health workers communicate with their families about avoiding transmission and allow them to see their loved ones. They listen more and view those they encounter as people first and patients second.
Health care directors also keep an eye out for locals whom they can train and mentor.
While the situation in North Kivu remains extremely challenging, there are some bright spots: In mid-April, the WHO reported that the experimental rVSV-ZEBOV-GP Ebola vaccine was 97.5% effective, meaning that it had probably saved thousands of lives. Health workers have administered the vaccine using a “ring vaccination” strategy, giving it to those determined to be at highest risk, such as contacts of people with Ebola and health workers.

Bausch has continuously voiced the need to view Ebola and other diseases not only as contagions to be stomped out but also as symptoms of extreme global inequality. He views people living in affected countries as essential partners in treating their compatriots and works to help them live in vastly improved, healthier circumstances with the capacity to address outbreaks on their own.
“Ebola is a scary, fascinating, terrible thing, and I’ve engaged with it directly and indirectly,” he says. “What I and others need to work toward is not only an on-the-ground response — which is obviously super important — but also, where does this come from? Why do we have this disease that seems to afflict only the poorest populations in the world? It’s not random who gets a communicable disease. There are many social, political, environmental and economic factors. Ebola is the canary in the coal mine signaling the world’s most vulnerable populations, people whose human right to health hasn’t been assured.”
The situation in North Kivu is especially complicated because of the region’s abundance of minerals, such as gold, tungsten and uranium, which are highly prized by the global technology and defense industries. Despite such riches, many towns in the area lack centralized electricity and water, internet and paved roads. Because the Congolese government is largely absent, residents rely on NGOs for basic health care and infrastructure.
When Ebola hits, responders try to stem disease transmission by sending out workers who conduct “contact tracing” — investigating suspected cases of Ebola in people’s homes and then tracking down all the people they interacted with in order to get them into isolation and care if they fall sick and vaccinate them. Ideally, investigators would visit all contacts every day for 21 days to check for early symptoms, something that is virtually impossible in the chaos of northeastern Congo today. Yet, every missed diagnosis can result in dozens or hundreds of additional cases.
If the person has already died, helping the family safely prepare the body for burial is crucial. Workers must walk a fine line between respecting cultural customs while also minimizing transmission. Investigators advise family members not to touch or kiss their loved ones, because bodily fluids on dead bodies are laden with the virus. To make matters worse, teams of workers must also decontaminate dwelling places with chlorine. But some property, such as mattresses, needs to be destroyed, which can further alienate the community.
Deep suspicions on the part of the Congolese make sense to Lina Moses, an assistant professor at Tulane University’s School of Public Health and Tropical Medicine, who has worked with Bausch on many outbreaks.
“People in West Africa and the Congo are dying all the time from many different things — starvation, violence, other diseases — and the international community doesn’t seem to care,” she explains. “But then there’s one case of Ebola, and everyone descends on the village. This has bred mistrust of outsiders, even people from [Congo’s capital] Kinshasa. I’ve never seen any response by local communities that seemed to me irrational if you understand the context.”
Although Bausch says the security situation in North Kivu is the most challenging he’s faced, the virologist says he and colleagues have encountered strong community resistance before. And there has also been chilling violence. He points out that in 2003, Congolese villagers beat and stoned to death four teachers who they accused of casting an evil spell to cause an Ebola outbreak.
And then there was the 2013–16 West African outbreak, where the international response was slow and lacked enough resources to battle the virus effectively. At one point in Sierra Leone, Bausch and one other colleague from the WHO, both wearing heavy protective gear in the stifling heat, did their best to manage about 60 patients. By then, all the nurses had died or fled in fear, leaving behind a facility bereft of support. It was, he says, the hardest situation he’s ever been in.
One moment from that time still haunts him. He had walked into an intake room where there were three beds crowded with people who had recently staggered in with symptoms of Ebola. On one mattress, a young girl who looked about 8 years old was already dead.
The only thing that Bausch knew about the girl was that she had come to the treatment center alone, and that broke his heart. He suspected that the rest of her family had already died, and he imagined her excruciating last moments.
“She reminded me of my own daughter, who was the same age at the time,” Bausch recalls. “I thought about all the horror this girl had endured, coming on her own from what must have been a terrifying situation at home to a hospital with such a strange and fearful environment, full of strange white people like myself wearing masks and gowns, and put onto a bed where other people were sick and bleeding.”
Whenever possible, Bausch tries to connect with people on a personal level and is known for being open and friendly with locals and co-workers alike. Nahoko Shindo, a disease expert at the WHO, remembers the first time she worked with Bausch in Sierra Leone and Guinea during an outbreak of Lassa fever. “It was difficult at first to know what to make of him,” she says, laughing. “When I first met him, he was wearing very bright African clothing made by local tailors. That impressed me. He was not your typical American.”
Another colleague, Stuart Nichol, chief of the Viral Special Pathogens Branch at the CDC, recalls Bausch’s remarkable work during a Lassa fever outbreak in Guinea, where he set up a field lab and collected rodents to test for infections, to better understand the transmission of Lassa virus, which is maintained in rodents and sometimes transmitted to humans through rodent consumption. “While he was managing research teams, he was also trapping, freezing and shipping these biospecimens to CDC labs in Atlanta for further analysis,” Nichol says. “And he was trying to get solar panels placed on the lab’s roof to generate more energy. Most clinicians wouldn’t be doing that. He has always been willing to get his hands dirty and do what needed to be done.”

Two intertwined pursuits have run throughout Bausch’s career. As a scientist, he is an expert in Ebola and other dangerous diseases such as Lassa fever, Marburg hemorrhagic fever and SARS (or severe acute respiratory syndrome), among many others. He took the directorship of UK-PHRST, he says, because it combines his three top interests: to help build the capacity of countries to internally address disease outbreaks, to participate in outbreak responses and to conduct research.
It’s important to Bausch to be both a good scientist and an activist. He met his wife and fellow infectious disease specialist, Frederique Jacquerioz, in Chiapas, Mexico, where the two were working on health and human rights projects in 1994, with Jacquerioz providing medical care to indigenous Mayan populations and Bausch working against unfair socioeconomic conditions with a nonprofit he had co-founded, Doctors for Global Health. She later helped train aid workers during an Ebola outbreak in West Africa and now works in migrant health and tropical medicine at Geneva University Hospitals in Switzerland. (The couple and their two children are based in Geneva, and Bausch commutes regularly to London.)
Bausch was a psychology major at Northwestern, focusing on neuroscience. After graduation he spent two years doing neuroscience research before entering medical school. Although initially headed toward a career in neurosurgery, he had a growing interest in the broader issues of health and human rights that led him to pursue training in internal medicine, infectious diseases and public health.
While Bausch continues leading aid responses all over the world, he holds onto a concept that came to him in the aftermath of the West African Ebola outbreak — a sort of contemporary post–World War II Marshall Plan for disease-ravaged countries.
“If you look at Europe today, it’s a pretty nice place,” he observes. “But if you were there in 1945, you might have said it would be impossible to achieve that level of prosperity. The measure of calamity in West Africa was on the order of the destruction of Europe. But if we put the same effort into rebuilding West Africa and other places like the Congo, as we did in Europe, 50 years from now, they could be equally economically stable and peaceful.”
Bausch and his colleagues are doing everything in their power to work toward that goal, one outbreak at a time. As Lina Moses notes, “Dan has helped our field move beyond simply using medical countermeasures such as vaccines, therapeutics and diagnostics. Now we know the only way to win these battles is to work with the community and have the community be part of the response.”
Lisa Stein ’94 MS is a freelance writer based in Evanston.
Tell us what you think of Northwestern Magazine in a short online survey by Aug. 15, and you’ll be entered to win one of eight $25 Amazon gift cards.
Reader Responses
No one has commented on this page yet.
Submit a Response