Flipping the Switch
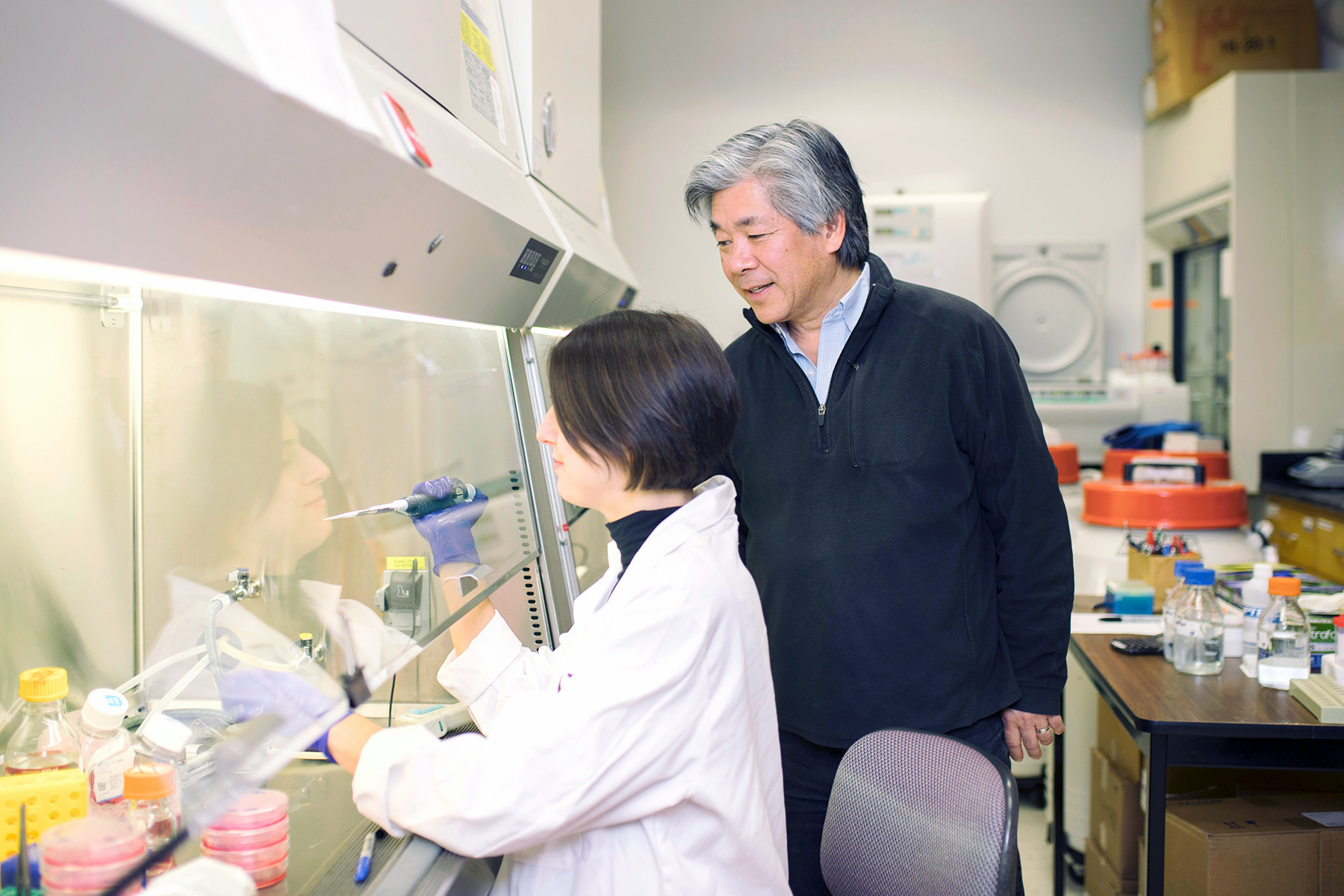
Morimoto is now focused on better understanding how the body’s quality control machinery keeps itself robust, and why it can fail in our later years. He’s determined to identify the first sign of failure in hopes of identifying who’s at risk and delaying the onset of Alzheimer’s disease.
Morimoto and his team have identified one important clue: When model organisms reach reproductive maturity, the quality control system shuts off genetically, marking the start of cellular aging.
“It’s like someone threw the switch,” he says. “But here’s the good news: We discovered we could turn the switch back on, and protein misfolding is suppressed.”
In subsequent work, the researchers identified 18 genes involved in this age-related neurodegeneration. By pinpointing the events — at the protein and genetic level — that lead to Alzheimer’s and other neurodegerative diseases, Morimoto says it may be possible to predict and even prevent protein misfolding.
“If we can predict who will get Alzheimer’s, we’ll know what to look for in the development of therapeutics,” he says. “Instead of waiting for the person to respond cognitively, which could take months, we’ll be able to monitor the changes at the cellular and molecular level to see if the therapeutic is working.”
Morimoto is now leading a national effort to better understand the role of protein quality control in neurodegenerative diseases — including Alzheimer’s — and human aging. Supported by a $12.6 million grant from the National Institute on Aging at the National Institutes of Health (NIH), researchers from Northwestern, Stanford University, Harvard Medical School, Scripps Research and the Gladstone Institutes at University of California, San Francisco, will use Morimoto’s concept of proteostasis to better understand the cellular and molecular changes that put older people at risk for Alzheimer’s and other diseases.
“We are bringing together all of the models and molecules that have ever been found to affect proteins and their stability,” Morimoto says. “We’re going to learn more about how cells deal with these different proteins, and new strategies for how to therapeutically reset the protein quality control system. I think ‘reset’ is the key word. The system is working wonderfully at 30 years old, at 20 years old. Let’s just reset it.”

Reader Responses
My brother was just diagnosed with ALS. He has had balance and walking challenges for a few months now. I presume this disease would also be impacted by protein misfolding. Would that a cure could be found, or at least his condition could be examined for this clue as well.
—Bill Yearout '75, Saint Louis, via Northwestern Magazine
No one has commented on this page yet.
Submit a Response